CHOOSING THERAPY FOR PCa
Thanks to the Michigan Urologist group MUSIC, there is a web-based tool that can let a man with early-stage prostate cancer see how thousands of other men in his situation have chosen to be treated - https://ask.musicurology.com/
ACTIVE SURVEILLANCE
One study showed significant anxiety for patients for the first 2 years, then reduced anxiety for active surveillance. (31) This study is a good review of how RP improves mortality compared to AS, WW. (34)
NONMETASTATIC PATIENTS
Risk of disease recurrence is comparable between RP and RT. Patients undergoing RP are at greater risk for incontinence and erectile dysfunction and decreased risk of bowel problems. The mortality rates following AS, RP and RT are comparable. (1) Surgical and radiation do not improve survival before 10 years of follow up compared to active surveillance for patients with early disease, but do reduce disease progression and development of metastatic disease PIVOT (10% vs. 5%) (5) and PROTECT (6% versus 2%) (5,6).
A study of low risk and very low risk patients showed that genomic scores are independent of tumor volume on prostate biopsy with 6-7% of patients being upgraded from low or very low risk classification based on genomic scores. (12)
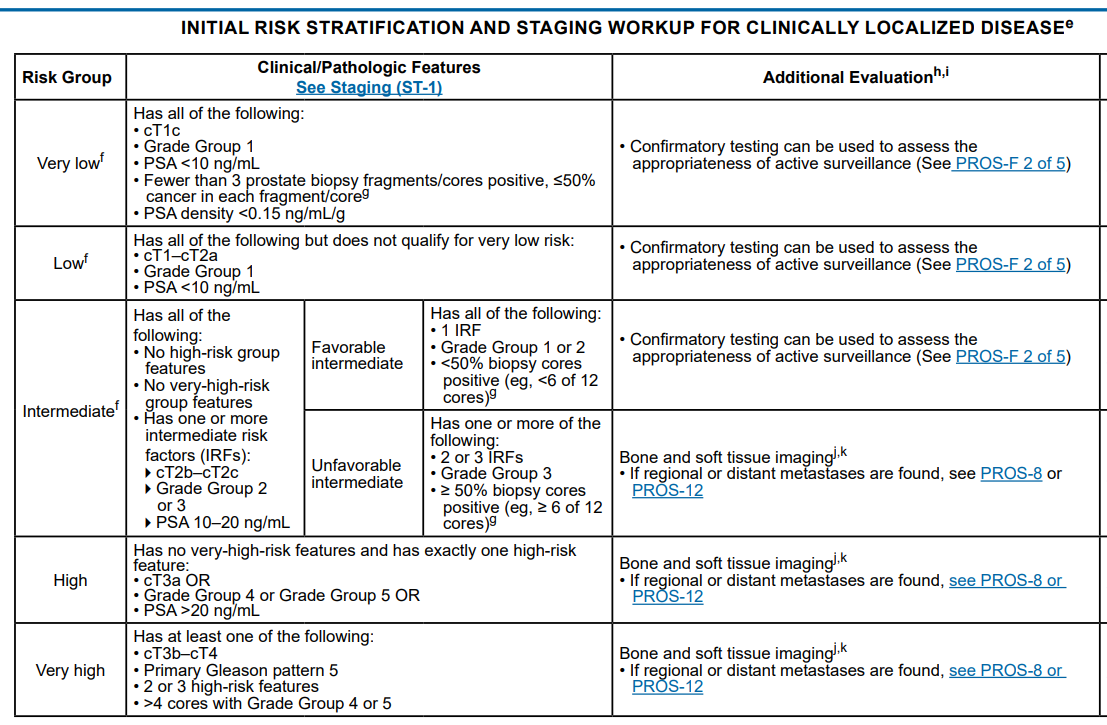
VERY LOW RISK
Metastatic progression rate of <1% at 15 years. (2,3,4) One large study reported in 2015 overall, cancer-specific, and metastasis-free survival rates of 93%, 99.9%, and 99.4%, respectively, at 10 years and 69%, 99.9%, and 99.4%, respectively, at 15 years. The cumulative incidence of grade reclassification was 26% at 10 years and was 31% at 15 years; cumulative incidence of curative intervention was 50% at 10 years and was 57% at 15 years. The median treatment-free survival was 8.5 years. (2) Gleason 3+3 has 3.9% rate of extracapsular extension and 14% of Gleason 3+4. (10)
LOW RISK
Studies suggest long term chance of metastasis or prostate cancer specific mortality on active surveillance occurrence to be roughly 3%. (8) 20% and 50% of PIVOT and PROTECT patients who started on active surveillance received treatment within 10 years. (5,6) According to the AUA, low risk patients with risk factors for progression (perineural invasion, African American, family history or genetic predispotion to lethal or metastatic prostate cancer) can be treated with definitive therapy.
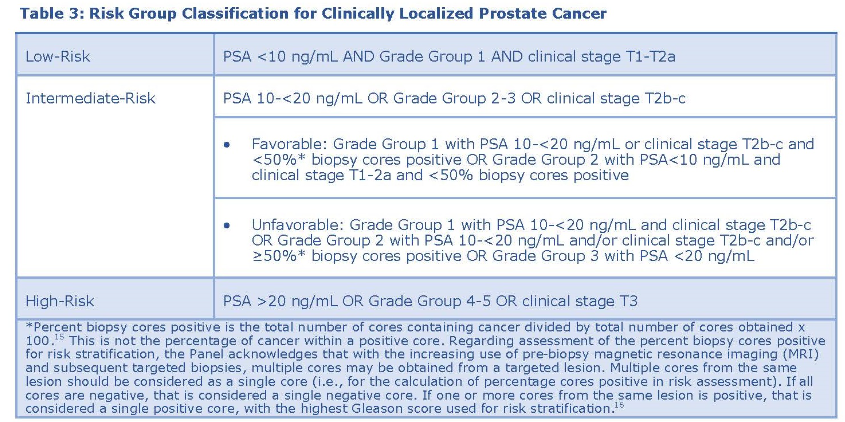
INTERMEDIATE RISK
PIVOT showed survival advantage for RP in intermediate risk patients. (8) At the 22.1 year follow up of the study, intermediate risk patients gained 2.1yrs on average OS after 13.6 in surgery cohort vs. 11.5 yrs observation. (35)
HIGH RISK
PIVOT showed lower rate of bone metastasis but not overall survival advantage with RP in high risk patients. (5) Gleason 9 and 10 treatment have been studied less extensively, a large retrospective 2018 study found that EBRT + BT boost + ADT was superior to RP or EBRT + ADT. (9) A study comparing 112 men w/ biopsy Gleason 10 showed 5yr OS was 80% for the RP group, 73% for the EBRT group, and 83% for the EBRT-BT group. The 5-year prostate CSS were 87%, 75%, and 94%, respectively. (13) In high risk PCA, up to 30% of patients will have occult LN metastasis foundon LN dissection, despite negative workup. (28,29) One retrospective study of SEER patients found high gleason score with low PSA had superior outcomes with RP compared to EBRT. (30)
LOCALLY ADVANCED OR REGIONALLY ADVANCED
Retrospective study of 13,856 men with T3‐T4N0M0 (LAPCa) or cT3‐T4N1M0 showed RP + XRT had higher 10yr CSS and OS compared to XRT + ADT. (14) Other studies have supported this. (15,16,17,18,19) Not everyone w/ PSM recurs and not everyone w/ biochemical recurrence progresses to clinical recurrence or death.
METASTASIS
Click here
AFRICAN AMERICANS
African American treated with sipuleucel-T had better outcomes than non-african americans. (36)
COUNSELING
Counseling patients can be difficult. A study of several hundred patients with PCa showed that 2/3 of them did not understand after counseling that the risk of disease recurrence is comparable between RP and RT. More than half did not comprehend that patients undergoing RP have greater risk for incontinence, ED and at decreased risk of bowel problems. (11) Using the P3P patient personal profile for prostate cancer can help make informed decisions.
COUNSELING - SIDE EFFECTS
A nice 2020 study of 2005 patients treated for PCa found that at 5 years for AS, RT, RP, ADT most functional differences between options attenuated by 5 years with RP having worse incontinence and sexual function at 5 years and gives an idea of the different side effects of each treatment. ~75% of the surgery patients underwent robotic surgery which contrasts to earlier studies looking at side effects with primary open surgeries. (33)
ACTIVE SURVEILLANCE
One study showed significant anxiety for patients for the first 2 years, then reduced anxiety for active surveillance. (31) This study is a good review of how RP improves mortality compared to AS, WW. (34)
NONMETASTATIC PATIENTS
Risk of disease recurrence is comparable between RP and RT. Patients undergoing RP are at greater risk for incontinence and erectile dysfunction and decreased risk of bowel problems. The mortality rates following AS, RP and RT are comparable. (1) Surgical and radiation do not improve survival before 10 years of follow up compared to active surveillance for patients with early disease, but do reduce disease progression and development of metastatic disease PIVOT (10% vs. 5%) (5) and PROTECT (6% versus 2%) (5,6).
A study of low risk and very low risk patients showed that genomic scores are independent of tumor volume on prostate biopsy with 6-7% of patients being upgraded from low or very low risk classification based on genomic scores. (12)
VERY LOW RISK
Metastatic progression rate of <1% at 15 years. (2,3,4) One large study reported in 2015 overall, cancer-specific, and metastasis-free survival rates of 93%, 99.9%, and 99.4%, respectively, at 10 years and 69%, 99.9%, and 99.4%, respectively, at 15 years. The cumulative incidence of grade reclassification was 26% at 10 years and was 31% at 15 years; cumulative incidence of curative intervention was 50% at 10 years and was 57% at 15 years. The median treatment-free survival was 8.5 years. (2) Gleason 3+3 has 3.9% rate of extracapsular extension and 14% of Gleason 3+4. (10)
LOW RISK
Studies suggest long term chance of metastasis or prostate cancer specific mortality on active surveillance occurrence to be roughly 3%. (8) 20% and 50% of PIVOT and PROTECT patients who started on active surveillance received treatment within 10 years. (5,6) According to the AUA, low risk patients with risk factors for progression (perineural invasion, African American, family history or genetic predispotion to lethal or metastatic prostate cancer) can be treated with definitive therapy.
INTERMEDIATE RISK
PIVOT showed survival advantage for RP in intermediate risk patients. (8) At the 22.1 year follow up of the study, intermediate risk patients gained 2.1yrs on average OS after 13.6 in surgery cohort vs. 11.5 yrs observation. (35)
HIGH RISK
PIVOT showed lower rate of bone metastasis but not overall survival advantage with RP in high risk patients. (5) Gleason 9 and 10 treatment have been studied less extensively, a large retrospective 2018 study found that EBRT + BT boost + ADT was superior to RP or EBRT + ADT. (9) A study comparing 112 men w/ biopsy Gleason 10 showed 5yr OS was 80% for the RP group, 73% for the EBRT group, and 83% for the EBRT-BT group. The 5-year prostate CSS were 87%, 75%, and 94%, respectively. (13) In high risk PCA, up to 30% of patients will have occult LN metastasis foundon LN dissection, despite negative workup. (28,29) One retrospective study of SEER patients found high gleason score with low PSA had superior outcomes with RP compared to EBRT. (30)
LOCALLY ADVANCED OR REGIONALLY ADVANCED
Retrospective study of 13,856 men with T3‐T4N0M0 (LAPCa) or cT3‐T4N1M0 showed RP + XRT had higher 10yr CSS and OS compared to XRT + ADT. (14) Other studies have supported this. (15,16,17,18,19) Not everyone w/ PSM recurs and not everyone w/ biochemical recurrence progresses to clinical recurrence or death.
METASTASIS
Click here
AFRICAN AMERICANS
African American treated with sipuleucel-T had better outcomes than non-african americans. (36)
COUNSELING
Counseling patients can be difficult. A study of several hundred patients with PCa showed that 2/3 of them did not understand after counseling that the risk of disease recurrence is comparable between RP and RT. More than half did not comprehend that patients undergoing RP have greater risk for incontinence, ED and at decreased risk of bowel problems. (11) Using the P3P patient personal profile for prostate cancer can help make informed decisions.
COUNSELING - SIDE EFFECTS
A nice 2020 study of 2005 patients treated for PCa found that at 5 years for AS, RT, RP, ADT most functional differences between options attenuated by 5 years with RP having worse incontinence and sexual function at 5 years and gives an idea of the different side effects of each treatment. ~75% of the surgery patients underwent robotic surgery which contrasts to earlier studies looking at side effects with primary open surgeries. (33)
RISK CALCULATORS
MSKCC
ERSPC
RPCRC, (20)
Finne, (22)
Chun, (21)
ProstataClass, (24)
Karakiewicz, (23)
Sunnybrook (26)
PCPT 2.0 (HG) (25)
P3P (32)
A head to head analysis of calculators for >7000 patients found no particular RC stands out when predicting biopsy outcome on the presence of any PCa. The ERSPC RPCRC is superior in identifying those men at risk for csPCa. Net benefit analyses show that a multivariate approach before further workup is advisable. (27)
MSKCC
ERSPC
RPCRC, (20)
Finne, (22)
Chun, (21)
ProstataClass, (24)
Karakiewicz, (23)
Sunnybrook (26)
PCPT 2.0 (HG) (25)
P3P (32)
A head to head analysis of calculators for >7000 patients found no particular RC stands out when predicting biopsy outcome on the presence of any PCa. The ERSPC RPCRC is superior in identifying those men at risk for csPCa. Net benefit analyses show that a multivariate approach before further workup is advisable. (27)
- Stam, Marie‐Anne, et al. "The accuracy of patients’ perceptions of the risks associated with localised prostate cancer treatments." BJU international 121.3 (2018): 405-414.
- Tosoian, Jeffrey J., et al. "Intermediate and longer-term outcomes from a prospective active-surveillance program for favorable-risk prostate cancer." Journal of Clinical Oncology33.30 (2015): 3379.
- Kasperzyk, Julie L., et al. "Watchful waiting and quality of life among prostate cancer survivors in the Physicians' Health Study." The Journal of urology 186.5 (2011): 1862-1867.
- Shappley III, William V., et al. "Prospective study of determinants and outcomes of deferred treatment or watchful waiting among men with prostate cancer in a nationwide cohort." Journal of Clinical Oncology 27.30 (2009): 4980.
- Hamdy, Freddie C., et al. "10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer." New England Journal of Medicine 375.15 (2016): 1415-1424.
- Wilt, Timothy J., et al. "Radical prostatectomy versus observation for localized prostate cancer." New England Journal of Medicine 367.3 (2012): 203-213.
- AUA Gudielines.Viewed May 10, 2018. http://www.auanet.org/guidelines/clinically-localized-prostate-cancer-new-(aua/astro/suo-guideline-2017)
- Klotz L, Vesprini D, Sethukavalan P et al: Long-term follow-up of a large active surveillance cohort of patients with prostate cancer.J Clin Oncol 2015; 33:272.
- Kishan, Amar U., et al. "Radical prostatectomy, external beam radiotherapy, or external beam radiotherapy with brachytherapy boost and disease progression and mortality in patients with Gleason score 9-10 prostate cancer." Jama319.9 (2018): 896-905.
- Hassan, Oudai, et al. "Incidence of Extraprostatic Extension at Radical Prostatectomy with Pure Gleason Score 3+ 3= 6 (Grade Group 1) Cancer: Implications for Whether Gleason Score 6 Prostate Cancer Should be Renamed" Not Cancer" and for Selection Criteria for Active Surveillance." The Journal of urology 199.6 (2018): 1482-1487.
- van Stam, Marie‐Anne, et al. "The accuracy of patients’ perceptions of the risks associated with localised prostate cancer treatments." BJU international 121.3 (2018): 405-414.
- Nyame, Yaw A., et al. "Genomic scores are independent of disease volume in men with favorable risk prostate cancer: implications for choosing men for active surveillance." The Journal of urology 199.2 (2018): 438-444.
- Sandler, K. A., et al. "Clinical Outcomes for Patients With Gleason Score 10 Prostate Adenocarcinoma: Results from a Multi-institutional Consortium Study." International Journal of Radiation Oncology• Biology• Physics 99.2 (2017): S132-S133.
- Jang, Thomas L., et al. "Comparative Effectiveness of Radical Prostatectomy With Adjuvant Radiotherapy Versus Radiotherapy Plus Androgen Deprivation Therapy For Men With Advanced Prostate Cancer. " Cancer. September 20, 2018.
- Ward JF, Slezak JM, Blute ML, Bergstralh EJ, Zincke H. Radical prostatectomy for clinically advanced (cT3) prostate cancer since the advent of prostate-specific antigen testing: 15-year outcome. BJU Int. 2005;95:751-756.
- Carver BS, Bianco FJ Jr, Scardino PT, Eastham JA. Long-term outcome following radical prostatectomy in men with clinical stage T3 prostate cancer. J Urol. 2006;176:564-568.
- Gerber GS, Thisted RA, Chodak GW, et al. Results of radical prostatectomy in men with locally advanced prostate cancer: multi-institutional pooled analysis. Eur Urol. 1997;32:385-390.
- Hsu CY, Joniau S, Oyen R, Roskams T, Van Poppel H. Outcome of surgery for clinical unilateral T3a prostate cancer: a single-institution experience. Eur Urol. 2007;51:121-128.
- Feldman AS, Meyer CP, Sanchez A, et al. Morbidity and mortality of locally advanced prostate cancer: a population based analysis comparing radical prostatectomy versus external beam radiation. J Urol. 2017;198:1061-1068.
- Roobol, Monique J., et al. "A risk-based strategy improves prostate-specific antigen–driven detection of prostate cancer." European urology 57.1 (2010): 79-85.
- Chun, Felix K-H., et al. "Development and internal validation of a nomogram predicting the probability of prostate cancer Gleason sum upgrading between biopsy and radical prostatectomy pathology." European urology 49.5 (2006): 820-826.
- Finne, Patrik, et al. "Algorithms based on prostate‐specific antigen (PSA), free PSA, digital rectal examination and prostate volume reduce false‐postitive PSA results in prostate cancer screening." International journal of cancer 111.2 (2004): 310-315.
- Karakiewicz, Pierre I., et al. "Development and validation of a nomogram predicting the outcome of prostate biopsy based on patient age, digital rectal examination and serum prostate specific antigen." The Journal of urology 173.6 (2005): 1930-1934.
- Stephan, Carsten, et al. "Multicenter evaluation of an artificial neural network to increase the prostate cancer detection rate and reduce unnecessary biopsies." Clinical chemistry 48.8 (2002): 1279-1287.
- Ankerst, Donna P., et al. "Prostate Cancer Prevention Trial risk calculator 2.0 for the prediction of low-vs high-grade prostate cancer." Urology 83.6 (2014): 1362-1368.
- Nam, Robert K., et al. "Assessing individual risk for prostate cancer." Journal of Clinical Oncology 25.24 (2007): 3582-3588.
- Pereira-Azevedo, Nuno, et al. "Head-to-head comparison of prostate cancer risk calculators predicting biopsy outcome." Translational andrology and urology 7.1 (2018): 18.
- Briganti, Alberto, et al. "Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores." European urology61.3 (2012): 480-487.
- Tosoian, Jeffrey J., et al. "Prediction of pathological stage based on clinical stage, serum prostate‐specific antigen, and biopsy Gleason score: Partin Tables in the contemporary era." BJU international 119.5 (2017): 676-683.
- Guo, Yadong, et al. “Survival Significance of Patients With Low Prostate-Specific Antigen and High-Grade Prostate Cancer After Radical Prostatectomy, External Beam Radiotherapy, or External Beam Radiotherapy With Brachytherapy.” Frontiers in Oncology, vol. 9, 2019.
- Marzouk, Karim, et al. “Long-Term Cancer Specific Anxiety in Men Undergoing Active Surveillance of Prostate Cancer: Findings from a Large Prospective Cohort.” The Journal of Urology, vol. 200, no. 6, 2018, pp. 1250–1255.
- https://www.p3p4me.org/
- Hoffman, Karen E., et al. "Patient-Reported Outcomes Through 5 Years for Active Surveillance, Surgery, Brachytherapy, or External Beam Radiation With or Without Androgen Deprivation Therapy for Localized Prostate Cancer." JAMA 323.2 (2020): 149-163.
- Kilpeläinen, Tuomas P., Petrus Järvinen, and Kari AO Tikkinen. "Randomized trials show a consistent benefit of radical prostatectomy on mortality outcomes." (2019): 1106-1108.
- Wilt, Timothy J., et al. "Radical Prostatectomy or Observation for Clinically Localized Prostate Cancer: Extended Follow-up of the Prostate Cancer Intervention Versus Observation Trial (PIVOT)." European urology (2020).
- Sartor, Oliver, et al. "Survival of African-American and Caucasian men after sipuleucel-T immunotherapy: outcomes from the PROCEED registry." Prostate Cancer and Prostatic Diseases (2020): 1-10.